GABA reuptake inhibitor
This article needs additional citations for verification. (October 2009) |
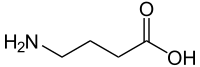
A GABA reuptake inhibitor (GRI) is a type of drug which acts as a reuptake inhibitor for the neurotransmitter gamma-Aminobutyric acid (GABA) by blocking the action of the gamma-Aminobutyric acid transporters (GATs). This in turn leads to increased extracellular concentrations of GABA and therefore an increase in GABAergic neurotransmission.[1] Gamma-aminobutyric acid (GABA) is an amino acid that functions as the predominant inhibitory neurotransmitter within the central nervous system, playing a crucial role in modulating neuronal activity in both the brain and spinal cord.[2] While GABA predominantly exerts inhibitory actions in the adult brain, it has an excitatory role during developmental stages.[3] When the neuron receives the action potential, GABA is released from the pre-synaptic cell to the synaptic cleft. After the action potential transmission, GABA is detected on the dendritic side, where specific receptors collectively contribute to the inhibitory outcome by facilitating GABA transmitter uptake. Facilitated by specific enzymes, GABA binds to post-synaptic receptors, with GABAergic neurons playing a key role in system regulation.[4] The inhibitory effects of GABA diminish when presynaptic neurons reabsorb it from the synaptic cleft for recycling by GABA transporters (GATs).[5] The reuptake mechanism is crucial for maintaining neurotransmitter levels and synaptic functioning.[6] Gamma-aminobutyric acid Reuptake Inhibitors (GRIs) hinder the functioning of GATs, preventing GABA reabsorption in the pre-synaptic cell. This results in increased GABA levels in the extracellular environment, leading to elevated GABA-mediated synaptic activity in the brain.[7][8]
Gamma-aminobutyric acid (GABA), the brain's main inhibitory neurotransmitter, plays a crucial role in regulating neuronal activity by dampening down neuron firing. Disruptions in GABAergic neurotransmission, such as reduced synthesis, reuptake dysfunction, or receptor abnormalities, can lead to various pathologies in the central nervous system, including epilepsy, anxiety disorders, Parkinson's disease, and sleep disorders. [9][10][11] The inhibitory neurotransmitter GABA plays a complex role in modulating anxiety and stress, regulating sleep, circadian rhythms, mood, cognition, and perception. Low GABA levels are associated with emotional and behavioral disruptions, including short-term and/or long-term stress, anxiety disorders, and sleep disorders.[12]
Indications
[edit]GRIs may be used in the clinical treatment of seizures, convulsions, or epilepsy as anticonvulsants/antiepileptics, depression,[13] anxiety disorders[11] such as generalized anxiety disorder (GAD), social phobia (SP) also known as social anxiety disorder (SAD), and panic disorder (PD) as anxiolytics, insomnia as hypnotics, muscle tremors or spasms as muscle relaxants, and chronic pain as analgesics. They may also potentially be used as anesthetics in surgery.
Effects
[edit]This section needs additional citations for verification. (March 2016) |
GRIs can induce a wide range of psychological and physiological effects, including:
- general and subjective alteration in consciousness
- dizziness
- blurry vision
- diplopia or double vision
- nystagmus or involuntary eye movements
- amblyopia or "lazy eye"
- tinnitus or "ear ringing"
- sedation
- drowsiness or somnolence
- narcolepsy
- tiredness or weakness
- fatigue or lethargy
- aches and pains
- headache
- nausea and vomiting
- gastrointestinal disturbances
- shakiness
- disorientation
- diminished awareness
- impaired attention
- focus and concentration
- decreased drive and motivation
- stuttering and slurring of speech
- confusion
- cognitive and memory impairment
- mood lift or drop
- depression
- anxiolysis
- disinhibition
- stress reduction
- euphoria or dysphoria
- irritability
- aggression
- anger or rage
- increased appetite and subsequent weight gain
- ataxia or impaired coordination and balance
- muscle relaxation
- trembling or muscle tremors and spasms
- paresthesia or "pins and needles"
- analgesia
- respiratory depression
- dyspnea or shortness of breath
Many of these properties are dependent on whether the GRI in question is capable of crossing the blood-brain-barrier (BBB). Those that do not will only produce peripheral effects.
GRIs such as CI-966 have been characterized as hallucinogens with effects analogous to those of the GABAA receptor agonist muscimol (a constituent of Amanita muscaria (fly agaric) mushrooms) when administered at sufficient doses.[14]
Tiagabine is another GRI that selectively inhibits the action of GABA reuptake and its mechanism of action is the same as selective serotonin reuptake inhibitor (SSRI).[11] It is used as a treatment for partial seizures in adults and children over 12, and works by amplifying GABA's calming effects in the brain. This, however, comes with potential drawbacks. While generally well-tolerated, some users experience concentration issues, language difficulties, and even a higher risk of depression, hallucinations, and paranoia.[15]
Overdose
[edit]At very high doses characterized by overdose, a number of symptoms may come to prominence, including:
- severe cognitive deficit to the point of acute retardation
- anterograde or retrograde amnesia
- drooling
- piloerection or "goose bumps"
- agitation or restlessness
- flailing
- thrashing and screaming
- unintentional or accidental injury
- delirium
- hallucinations
- myoclonus
- dystonia
- paralysis
- stupor
- faintness or loss of consciousness
- seizures or convulsions
- status epilepticus
- coma and respiratory arrest or cessation of breathing
- brain damage
- death
List of GRIs
[edit]- CI-966[16]
- Deramciclane (EGIS-3886)
- Gabaculine
- Guvacine (C10149)
- Nipecotic acid
- NNC 05-2090
- NNC-711[16]
- SKF-89976A[16]
- SNAP-5114
- Tiagabine (Gabitril)[16]
- Hyperforin[17]
- Arecaidine
See also
[edit]References
[edit]- ^ Bauer J, Cooper-Mahkorn D (2008-08-08). "Tiagabine: efficacy and safety in partial seizures – current status". Neuropsychiatric Disease and Treatment. 4 (4): 731–736. doi:10.2147/NDT.S833. PMC 2536540. PMID 19043517.
- ^ Jewett BE, Sharma S (2024), "Physiology, GABA", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 30020683, retrieved 2024-02-15
- ^ Allen MJ, Sabir S, Sharma S (2024), "GABA Receptor", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 30252380, retrieved 2024-02-15
- ^ Gottlieb DI (1988). "GABAergic Neurons". Scientific American. 258 (2): 82–89. Bibcode:1988SciAm.258b..82G. doi:10.1038/scientificamerican0288-82. ISSN 0036-8733. JSTOR 24988982. PMID 2847312.
- ^ Olsen RW, DeLorey TM (1999), "GABA Synthesis, Uptake and Release", Basic Neurochemistry: Molecular, Cellular and Medical Aspects. 6th edition, Lippincott-Raven, retrieved 2024-02-15
- ^ Salters-Pedneault, K. (2023, June 13). How selective serotonin reuptake inhibitors (ssris) works. Verywell Mind.
- ^ Zafar S, Jabeen I (2018). "Structure, Function, and Modulation of γ-Aminobutyric Acid Transporter 1 (GAT1) in Neurological Disorders: A Pharmacoinformatic Prospective". Frontiers in Chemistry. 6: 397. Bibcode:2018FrCh....6..397Z. doi:10.3389/fchem.2018.00397. ISSN 2296-2646. PMC 6141625. PMID 30255012.
- ^ Niessen WM (2020-10-01). "Interpretation of tandem mass spectra of antiepileptic drugs using accurate-m/z data and m/z-shifts with stable-isotope labeled analogues". International Journal of Mass Spectrometry. 456: 116409. Bibcode:2020IJMSp.456k6409N. doi:10.1016/j.ijms.2020.116409. ISSN 1387-3806. S2CID 224856466.
- ^ Perucca E, Bialer M, White HS (2023-09-01). "New GABA-Targeting Therapies for the Treatment of Seizures and Epilepsy: I. Role of GABA as a Modulator of Seizure Activity and Recently Approved Medications Acting on the GABA System". CNS Drugs. 37 (9): 755–779. doi:10.1007/s40263-023-01027-2. ISSN 1179-1934. PMC 10501955. PMID 37603262.
- ^ Motiwala Z, Aduri NG, Shaye H, Han GW, Lam JH, Katritch V, Cherezov V, Gati C (2022). "Structural basis of GABA reuptake inhibition". Nature. 606 (7915): 820–826. Bibcode:2022Natur.606..820M. doi:10.1038/s41586-022-04814-x. ISSN 1476-4687. PMC 9394549. PMID 35676483.
- ^ a b c Loughlin, K. R., Generali, J. A. (2006). The Guide to Off-label Prescription Drugs: New Uses for FDA-approved Prescription Drugs. United Kingdom: Free Press.
- ^ Hepsomali P, Groeger JA, Nishihira J, Scholey A (2020). "Effects of Oral Gamma-Aminobutyric Acid (GABA) Administration on Stress and Sleep in Humans: A Systematic Review". Frontiers in Neuroscience. 14: 923. doi:10.3389/fnins.2020.00923. ISSN 1662-453X. PMC 7527439. PMID 33041752.
- ^ Zanoli P (2004). "Role of Hyperforin in the Pharmacological Activities of St. John's Wort". CNS Drug Reviews. 10 (3): 203–218. doi:10.1111/j.1527-3458.2004.tb00022.x. ISSN 1080-563X. PMC 6741737. PMID 15492771.
- ^ Hollister LE (1990). "New class of hallucinogens: GABA-enhancing agents". Drug Development Research. 21 (3): 253–256. doi:10.1002/ddr.430210311. ISSN 0272-4391. S2CID 143868762.
- ^ Cavanna, A. E., Ali, F., Rickards, H. E., & McCorry, D. (2010). Behavioral and cognitive effects of anti-epileptic drugs. Discovery medicine, 9(45), 138–144.
- ^ a b c d Borden LA, Murali Dhar TG, Smith KE, Weinshank RL, Branchek TA, Gluchowski C (1994). "Tiagabine, SK&F 89976-A, CI-966, and NNC-711 are selective for the cloned GABA transporter GAT-1". Eur J Pharmacol. 269 (2): 219–224. doi:10.1016/0922-4106(94)90089-2. PMID 7851497.
- ^ Wonnemann M, Singer A, Müller WE (August 2000). "Inhibition of Synaptosomal Uptake of 3H-L-glutamate and 3H-GABA by Hyperforin, a Major Constituent of St. John's Wort The Role of Amiloride Sensitive Sodium Conductive Pathways". Neuropsychopharmacology. 23 (2): 188–197. doi:10.1016/S0893-133X(00)00102-0. PMID 10882845.
- Carlson NR, Birkett M (2017). Physiology of Behavior (12 ed.). Pearson. p. 103. ISBN 9780134320823.
